

MS NOW OPINION
Understand Today’s News

Kamala Harris needs to do better than this
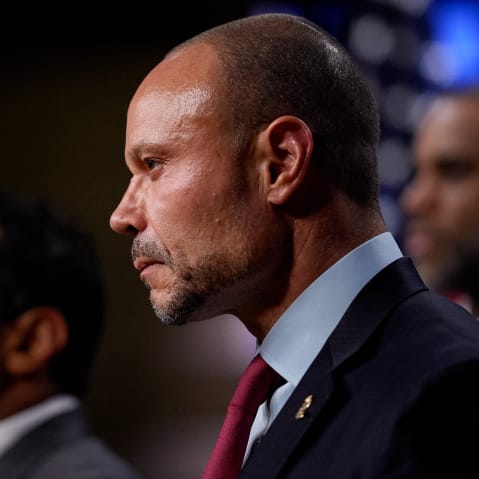
Kaivan Shroff
Like this content? Follow our rundown delivered daily right to your inbox
Shows
Know Your Value
Latest from MS NOW
Maddowblog
Monday’s Mini-Report, 2.9.26
Deadline: Legal Blog